Healthcare comes home
Posted on 13 June 2023
Modern health services are determined to put the patient in control of their own healthcare journey, and they’re looking for new technologies to help them do it.

Professor Krauss with the blood-testing device, designed to be self-administered and used in the home.
What’s really powerful is that all of this is only just beginning to happen, so the NHS isn’t entirely sure how far they can take the concept of a ‘virtual ward’... So I see a real opportunity here: if we get the timing right, we could help to shape their policy.
So for healthcare organisations across the world, including our own National Health Service, the opportunity to enable patients to take a highly accurate blood test without leaving their own home, is a highly attractive proposition.
Professors Thomas Krauss and Steve Johnson of our School of Physics, Engineering and Technology are leading a team which can help make that goal a reality. They’ve created a device which can fit into the palm of a hand, deliver “gold-standard laboratory accuracy” and cost only a few pounds to manufacture. And the entire blood testing process could be self-administered at home.
At their laboratory in Campus West, Krauss and Johnson demonstrate a small device, not unlike something Apple might have designed in the early days of the iPod, and a cartridge which looks identical in size and appearance to the Covid-19 self-testing kits everyone used during the pandemic.
“The user squeezes a drop of blood into the cartridge, which then moves up through the sensing devices using capillary action,” says Professor Krauss as he explains how the cartridge is placed into the reader to give the patient their specific result, which can then be passed onto clinical staff.
He explains that the device reads a panel of blood-borne protein biomarkers and that many diseases, including heart disease, kidney disease, immunodeficiencies and blood infections all reveal themselves by altering such protein biomarkers, which the device can be sensitised to pick up.
The team are well aware that similar blood-reading devices already exist, but Professor Krauss says that they can’t compete with the York technology for accuracy in relation to cost.
“Our accuracy is as high as the laboratory gold standard, and while other manufacturers can offer similar results, they can’t do it for the cost we can. Our devices can be injection moulded and only require very simple optical components, meaning that they can be manufactured for a few pounds. We’re able to offer this accuracy at a very low cost, such that every patient can afford it
The technology has recently received patent protection and the team have now formed a company, Phorest Diagnostics, to take the technology to the market. They are currently recruiting a management team with a view to marketing the device and moving it to the clinical trials stage.
And their timing may be opportune. The NHS is expanding its ‘virtual ward’ initiative - a drive to deliver as many services as possible in the home - and the York technology could become a major part of that. Thomas and Steve’s team are well connected to some of the leaders tasked with implementing the still-developing NHS virtual ward vision, so they are well placed to make an impact.
“What’s really powerful is that all of this is only just beginning to happen, so the NHS isn’t entirely sure how far they can take the concept of a ‘virtual ward’; they know they can do standard things, like taking blood pressure and cholesterol, at home, but they don’t yet know the full potential of a virtual ward because a lot of technology they would like to use doesn’t yet exist. So I see a real opportunity here: if we get the timing right, we could help to shape their policy.”
But the real benefit, he says, is to the patient. People using the device are likely to be severely immunosuppressed, meaning they’re unable to fight even minor infections. So avoiding exposure to germs, unavoidably present in hospital and GP surgeries, is a huge advantage.
“I was talking to a patient just the other day,” says Professor Krauss. “I was asking him whether the technology should work with iPhones and all sorts of other technical questions. He told me ‘I don’t care. I’m arthritic and I need blood tests every month. My immune system is weak and I don’t want to go out. If you can find a way for me to have a blood test without leaving the house - that would be amazing. That’s all I want’.”
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.

Thomas Krauss
Research Title: Professor of Photonics, School of Physics, Engineering and Technology.

Steven Johnson
Research Title: Head of Intelligent Systems and Nano-science Research Group.
Explore more research
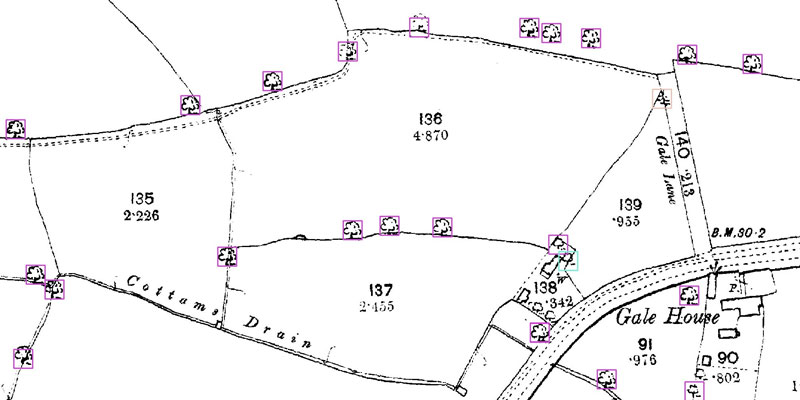
A research project needed to spot trees on historic ordnance survey maps, so colleagues in computer science found a solution.

We’re using gaming technology to ensure prospective teachers are fully prepared for their careers.

A low cost, high-accuracy device, could play a large part in the NHS's 'virtual wards'.
