Depression and the Third Age
-
Research
- Health and Wellbeing
Posted on 6 January 2015
Research on depression in older people by Simon Gilbody and his team is now influencing policymakers and practitioners in this often neglected but hugely important field of health care.

If you have cancer the prognosis is much worse if you have a concurrent psychological disorder.
As a trained psychiatrist and psychological therapist who describes himself as 'man and boy' a creature of the NHS, Professor Simon Gilbody brings a wealth of front line clinical experience to his role as Director of the York Mental Health and Addictions Research Group.
“I suppose I am unusual in that I had a proper job before becoming an academic,” Professor Gilbody laughs, before excitedly listing the number of his major long-term publicly funded projects that are now coming to fruition.
As a Medical Research Council-trained population scientist, he came to the University of York’s Department of Health Science a little more than a decade ago and began to build a group that now boasts 35 full time staff. “It started as myself and an administrator,” he says, “Now we are running some of the biggest publicly-funded research programmes in the NHS mental health sector.”
Mental health
Professor Gilbody explained that what was once seen as the Cinderella of the health service is increasingly becoming the focus of attention for policy makers and medical practitioners. “There are two key drivers for this change. The first is a hard-nosed assessment of the impact mental health problems are having on the economy. Official estimates suggest that as much as £26billion a year is lost to the economy as a result of these issues. That is a big number and the Treasury is belatedly taking notice,” he said.
The second driver is a growing understanding that many physical illnesses – and especially those associated with older age – also have an important psychological dimension. “We now know that when you get a long-term physical health problem the chances of you having a common mental disorder such as anxiety or depression are elevated by about three-fold,” he said.
“That is important for a number or reasons. If you have got ischemic heart disease, the chances of you dying in the next five years are elevated by about two-fold if you have a psychological illness along with it. Likewise, if you have cancer the prognosis is much worse if you have a concurrent psychological disorder. The NHS is recognising these problems and looking for the best ways to intervene.”
Which is where Professor Gilbody and his team at York come in: “Our Collaborative care in Screen-Positive Elder Research (CASPER) largely focuses on finding effective and efficient ways of delivering non-pharmacological treatment for common mental disorders such as depression and anxiety. But we are also looking at ways of improving the physical health and wellbeing of people with severe mental illness like schizophrenia.”
Talking therapies
He explained that one of the CASPER studies into the effectiveness of 'talking therapies' was producing analytical data that will help shape treatments, particular at GP level, that will benefit older people and offer an alternative or complement to less effective drug based solutions.
All too often he says mental health professionals and physicians within the NHS don’t talk to one another: “Facilitating some sort of conversation between them is one of our roles, along with trying to move doctors, nurses and people who work in the NHS out of a strong philosophical mind body dualism split, breaking down that split is important and that is a win-win if we can achieve that as our results show that physical conditions can improve through the provision of talking therapies.”
Professor Gilbody concluded that: “Here at York our researchers are producing an evidence-currency which trades very well in the NHS and which has the potential to change practice and policy right across the UK and internationally.”
The text of this article is licensed under a Creative Commons Licence. You're free to republish it, as long as you link back to this page and credit us.

Simon Gilbody
Research Title: Director of the Mental Health and Addictions Research Group (MHARG)
Professor Gilbody holds a joint appointment with the Hull York Medical School (HYMS), where he is a member of the Centre for Health and Population Sciences.
Discover the details
Find out more in the York Research Database
Projects
Article
Visit the departments
Explore more research
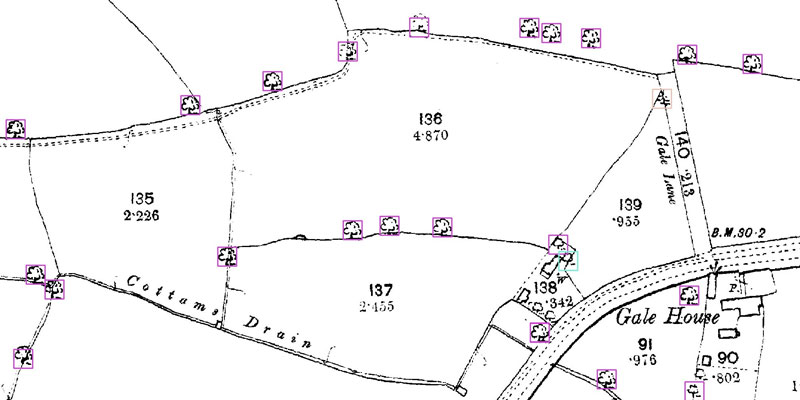
A research project needed to spot trees on historic ordnance survey maps, so colleagues in computer science found a solution.

We’re using gaming technology to ensure prospective teachers are fully prepared for their careers.

A low cost, high-accuracy device, could play a large part in the NHS's 'virtual wards'.
